Developing a Health Quality System Driven by Lay Health Workers in Botswana
Developing a Health Quality System Driven by Lay Health Workers in Botswana
Quality service delivery remains paramount despite shortages of human resources for health, particularly in low- and middle-income countries like Botswana. Efficient delivery of care remains below standard despite countrywide availability of HIV guidelines. Administrative and technical oversight at the district level is overseen by district health management teams supported by a technical program manager who is often overburdened by routine duties. The aim of this case study is to describe how integration of lay health workers into the healthcare system using a continuous quality improvement approach can improve service delivery outcomes.
Description: Using a continuous quality improvement approach, we monitored facility improvement using “core essential elements” (CEEs: defined as a set of tools used to assess and score facility support against an established standard). Three underperforming epidemic control indicators (linkage to treatment, viral load coverage and viral load suppression) were selected to be monitored for three months among six high-volume facilities supporting over 9,000 people living with HIV in two districts. A SIMS baseline assessment showed that 83% of facilities had a CEEs aggregate score below 80%, which was considered to be poor or implementing below set standards and guidelines. The lay health workers were trained to use a weekly SIMS-based service quality checklist for real time monitoring and remediation of the three indicators across all facilities. This ultimately improved program outcomes.
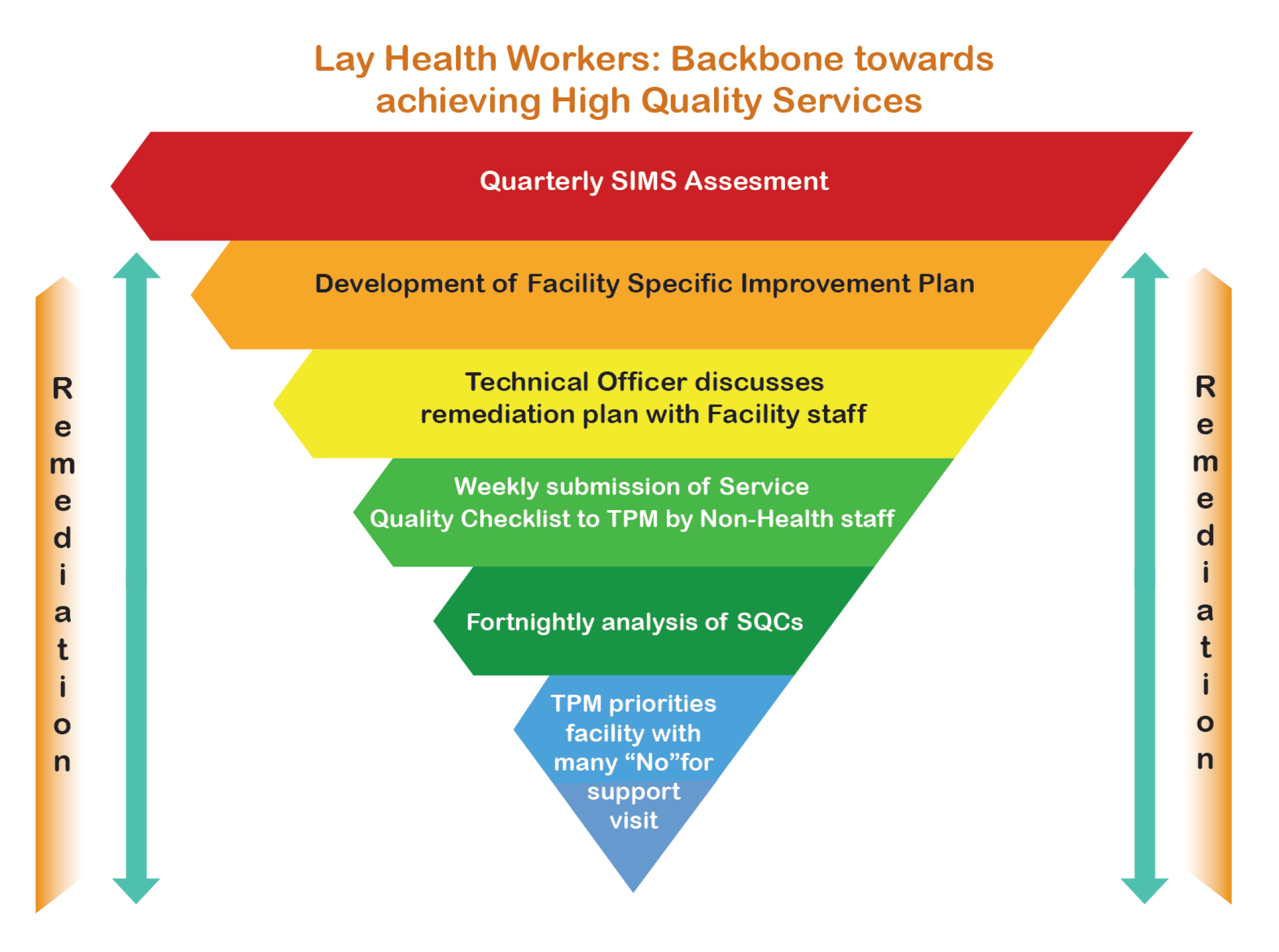
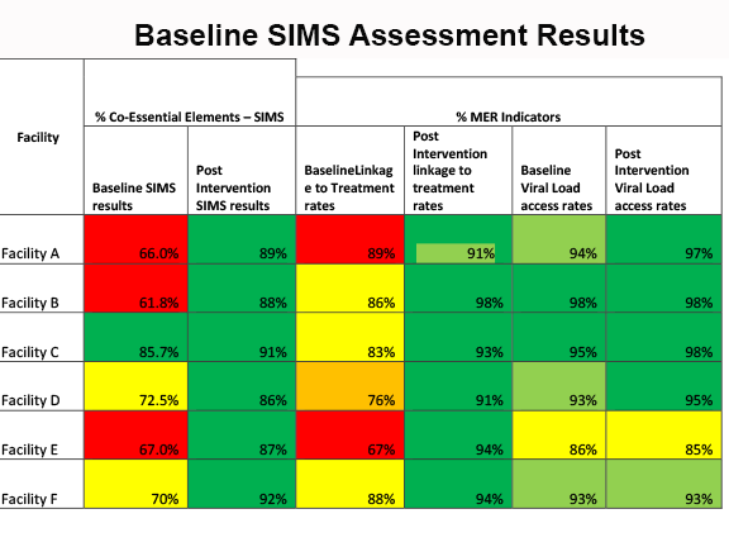
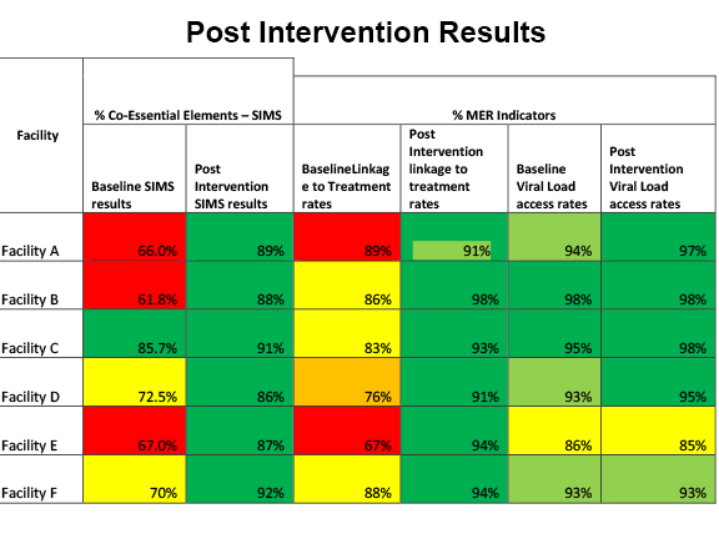
Lessons Learned: SIMS post remediation results revealed 100% of facilities had CEE scores above 80% and 100% of facilities achieving over 90% of key epidemic control targets. Due to these results, a service quality checklist comprised of key CEEs that assess implementation of standard operational plans, guidelines, and policies in HIV management was developed for lay health workers to monitor facilities and submit weekly reports to the technical program manager.
Conclusion/ Next Steps: Facility mentoring, training, and collaboration with lay health workers to improve quality of services can potentially result in HIV epidemic control and improved health service delivery and can support task shifting for improved client outcomes.


