Tuberculosis Testing
CQI Strategy Improves Tuberculosis Testing Among HIV Patients Attending Two Health Facilities in Tanga Region
Tuberculosis (TB) is highly endemic in Tanzania. To reduce the TB disease burden, case detection needs to be expanded. The TB cascade evaluation for people living with HIV (PLHIV) includes GeneXpert TB testing, which is the gold standard for TB testing. However, despite the availability of GeneXpert machines in facilities in Tanzania, testing of TB-presumptive PLHIV clients has remained suboptimal. We applied a quality improvement (QI) approach to increase the number of samples processed from TB-presumptive PLHIV and, in turn, optimized the utilization of GeneXpert machines. This analysis compares the percent of TB samples that were collected and tested before and after the intervention.
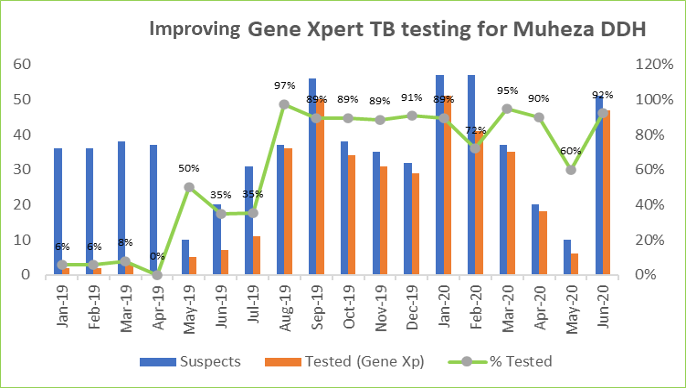
Muheza Designated District Hospital (DDH) Facility
Data from the Muheza DDH facility showed that between January and May 2019, an average of 17% of samples was collected and tested for TB among HIV positive clients attending the care and treatment clinics. Root cause analysis was performed on the data. The following gaps were identified: 1) TB samples from PLHIV were not ordered by the clinics, and clients were referred to the laboratory for sample collection and testing, 2) Not all clients who were asked to go to the laboratory went, and 3) There was poor documentation in TB-presumptive registers.
Based on these results, an intervention was designed to increase collection and testing. Instead of being referred to the laboratory, client samples were collected at the clinic. The triage nurse then delivered the sample to the testing laboratory. Finally, the data clerk ensured that all sample results were documented on the presumptive registers.
After the CQI intervention began in June 2019, the rate of sample collection and testing rose to an average of 82% between July 2019 and June 2020 (Figure 1).
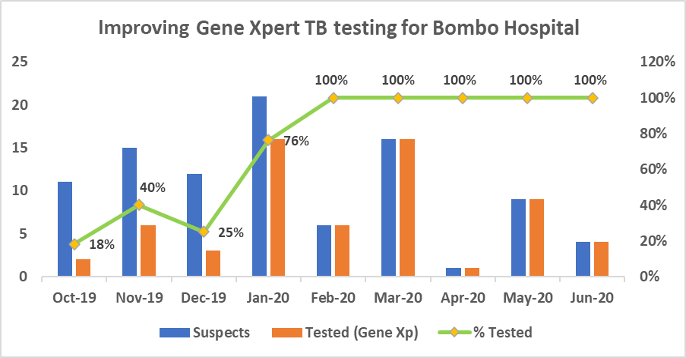
Bombo Referral Hospital
The success at the Muheza DDH led to the intervention being implemented at Bombo Referral Hospital, another large hospital in the area, whose December 2019 data review found a lonely 28% uptake for TB testing among HIV clients who had presumptive TB. Root cause analysis was done, and similar gaps as those in Muheza DDH were identified. The analysis identified that: 1) The clinics did not order TB samples from PLHIV, and clients were asked to go to the laboratory for sample collection and testing, 2) Clinic staff were not aware of the importance of using GeneXpert machines for testing TB presumptive clients, and 3) There was poor documentation in TB-presumptive registers.
The best practices protocol implemented at Muheza DDH were replicated at Bombo Hospital. Additionally, clinic staff were mentored on the importance of using GeneXpert machines for TB diagnosis of HIV clients who had presumptive TB.
Following the implementation of the protocol between January and June 2020, the facility saw an increase in the average percentage of samples tested from the baseline of 28% to 100% (Figure 2).
Figure 1. TB cascade evaluation at Muheza DDH
Figure 2. TB cascade evaluation at Bombo Hospital
Improvements with CQI
This CQI approach shows that TB testing for presumptive clients at healthcare facilities can be improved without additional resources and in a short time, only by making changes to protocol and measuring results. We have also learned that sample collection at the clinic will generate more samples and ensure all eligible clients are tested for TB.
Impact Story Written by Haji Msuya, Laboratory Advisor
Reviewed by Patience Komba, Associate Director Program Quality